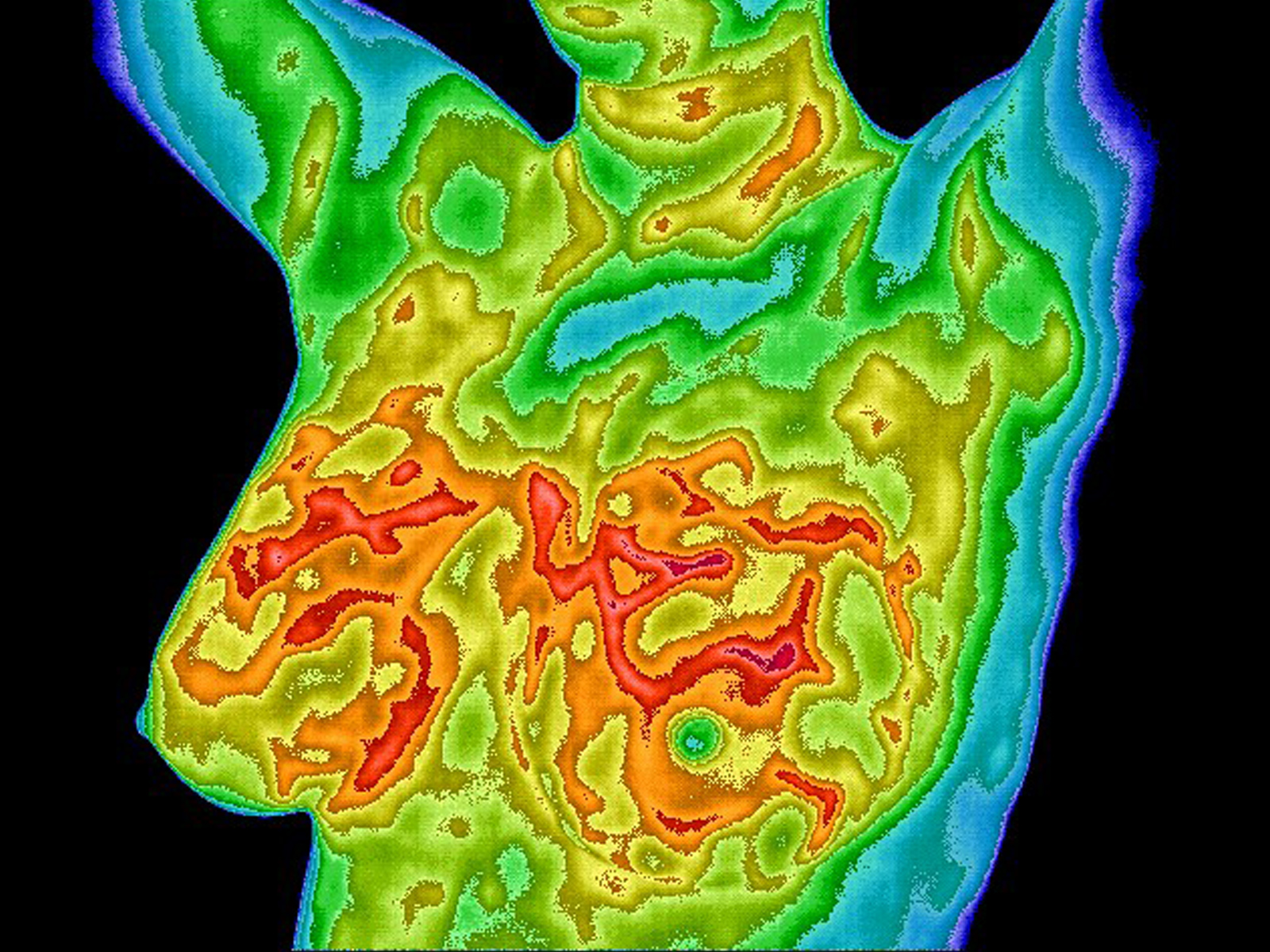
Breast thermography is an imaging method that uses sophisticated infrared cameras and computer systems to detect the heat given off of the surface of the skin. This heat is processed into a high-resolution image that may be analyzed for some of the earliest signs of breast cancer.
Breast thermography detects a process called neoangiogenesis, or new blood vessel formation. As pre-cancerous and cancerous cells grow and multiply they demand an increased blood supply to bring in nutrients and expel waste products. In order to do this the cells cause the growth of new blood vessels, which in turn causes increased heat that can be detected with breast thermography.
There are no harmful side effects associated with the test. Breast thermography uses no radiation or other invasive procedures. The imaging system detects only heat given off the body. There is no any discomfort for the woman being examined. The examination is completely comfortable since there is no contact with the breasts at all.
The procedure is pretty simple. First, the patient is given pre-examination preparation instructions to refrain from certain things before the exam. Then once they arrive, the patient fills out a breast health history form. Then the patient is lead to the imaging laboratory where strict temperature controls are in place. The patient is disrobed from the waist up and left to acclimate to the room temperature for 15 minutes. Then she is positioned in front of the IR camera where images are captured of the breasts from different angles. These strict protocols are in place to insure that the images are accurate representations of the patient’s underlying physiology.
Thermography is as different from mammography as apples and oranges. Thermography is an examination of physiology. It detects functional changes in the breast such as increased blood flow caused by pre-cancerous or cancerous cells. Mammography is a structural examination. It looks for structural changes such as the presence of an actual mass of cells. Each test is looking for completely different things. I think you can see that the two tests really shouldn’t be compared. The procedures complement each other, they don’t replace each other.
You may say to yourself why is it important to look at these functional heat changes as opposed to simply looking for a mass on a mammogram? This is one of the most exciting aspects of thermography. Most cancers take 8-10 years to grow to the size of a dime. Breast cancer research has shown that if a mass could be caught during the earliest part of its growth phase, 95% cure rates would be possible. In the majority of cases, temperature changes are seen on a breast thermogram long before a lump or mass can be detected.
You may ask if a woman, who has abnormal heat changes on a breast thermogram, could be at higher risk of future breast cancer? The answer is Yes! This is where thermography excels. One of breast thermography’s greatest advantages over other screening methods is the ability to warn women who are at the greatest potential risk for future breast cancer. You see, if we monitor these woman carefully we have the best chance of catching the cancer at its smallest size.
This is a method that could be used to screen younger women who have a family history of breast cancer or other risk factors. The literature notes that approximately 15% of breast cancers are occurring in women under 49, and this number is increasing. Unfortunately, currently there are no real imaging guidelines for screening women under age 40. Also, breast density at these younger ages cause problems when reading mammograms. However, breast density, implants, and breast size do not affect the interpretation of breast thermograms.
We recommend a baseline breast thermogram at age 20 with re-examinations about every 3 years to age 30 and annually after that. In this way we are able to provide screening for women at all ages. The images are analyzed for abnormalities and the results are added to the patient’s known risk factors to complete the picture. Information gained from over 30 years of research has shown that, in the absence of any other positive tests, an abnormal breast thermogram carries with it a 22x higher risk of future breast cancer. That’s a significant increase! Studies indicate that an abnormal breast thermogram is the highest known risk marker for the future development of breast cancer. An abnormal thermogram is 10x more significant a risk than a first order family history of the disease.
You may ask, with the prospect of identifying women at higher risk for breast cancer, what effect can breast thermography have on a woman’s ability to take action against this disease? This is the bottom line question. Since 1 in 8 women will get breast cancer in their lifetime, I feel that we must do everything we can to combat this condition. The risk for every woman is already too high. Studies have shown that when breast thermography is added to a woman’s regular breast health care, over 95% of very early stage cancers will be detected.
What this mean to a woman that has detected cancer this early? This translates, potentially, into 95% cure rates. Breast thermography is a very exciting technology which brings a great deal of good news to women.
Another role of thermography in addition to early detection is in prevention. The single greatest known risk factor for the development of breast cancer is lifetime exposure of the breasts to the hormone estrogen. As such, if we could warn a woman that her breasts were being exposed to more estrogen than normal would we be able to play a role in prevention? – I believe so. Estrogen in the breast causes an increase in the metabolism of the ductal cells. This increase in metabolism necessitates an increase in blood circulation in order to bring in nutrients and remove waste. On a thermogram this shows up as a unique blood vessel display across both breasts. When this is seen a woman is referred back to her doctor for more tests to determine if the levels of estrogen are abnormal, and if positive, what treatment is appropriate. In this role, thermography may play a very important part in prevention.
To give a brief history of thermography, In the mid 1970’s, the first large scale breast cancer screening research study, called the breast cancer detection and demonstration project, tested mammography, thermography, and physical examination of the breast. The question asked was whether or not thermography could replace mammography. You can see the flaw here; remember that the tests are completely different. The researchers were trying to use thermography like mammography to locate a mass in the breast, and not the early signs of pathology – where thermography excels. Also, the equipment used was designed for industrial purposes. These cameras used IR detectors that were not tuned to the IR wavelength given off by humans. Also, there was no computerized analysis available as there is today. No imaging protocols were used – there were no patient preparation instructions and no laboratory temperature controls. No one was trained to interpret or take the images. It wasn’t until the mid 1980’s that a fully established interpretation protocol was in place. As you can see, the study was seriously flawed in many areas. Since this study, significant advances in computerized medical infrared imaging have been made and over 800 index medicus studies have been performed confirming breast thermography as the earliest detector of breast cancer.
Considering all these protocols and special equipment, one would think that special qualifications are necessary to perform this procedure. To take the images, a person needs to be trained and board certified as a clinical thermographic technician. In order to read the images you need to be a licensed diagnostician, such as a DC, MD, or DO, and board certified as a clinical thermographer.
We know the FDA regulates mammography centers. You may think to yourself are there any standards for thermography? Yes there is. The FDA cleared Breast thermography for adjunctive breast cancer screening in 1982. And there are strict standards and guidelines for equipment, patient and laboratory protocols, and the interpretation of the images. This is why it is so important for patients to choose an imaging center with qualified personnel and equipment.It’s never too soon to start thinking about your breast health. If you or a woman you know is 20 years of age or older, now is the time to start thinking about early breast cancer detection. Breast Thermography is an amazing technology that may be used as a risk marker for early breast cancer detection. For a Free Consultation on Breast Thermography and how you can incorporate it into your breast care, contact Noushin Izadi at View of Health Thermography Clinic located at 1582 West San Marcos Blvd, Suite #103, San Marcos, Calif., by calling (262) 501-0349 or by email through the form here.